Have you ever wondered why some people suffer from chronic illnesses that seem to attack their own bodies? Autoimmune diseases are a group of disorders where the immune system mistakenly targets healthy tissues. This leads to inflammation and damage, affecting various parts of the body. Understanding these conditions is crucial for managing symptoms effectively and improving quality of life. Let’s delve into the complexities of autoimmune diseases, exploring their causes, symptoms, and treatments.
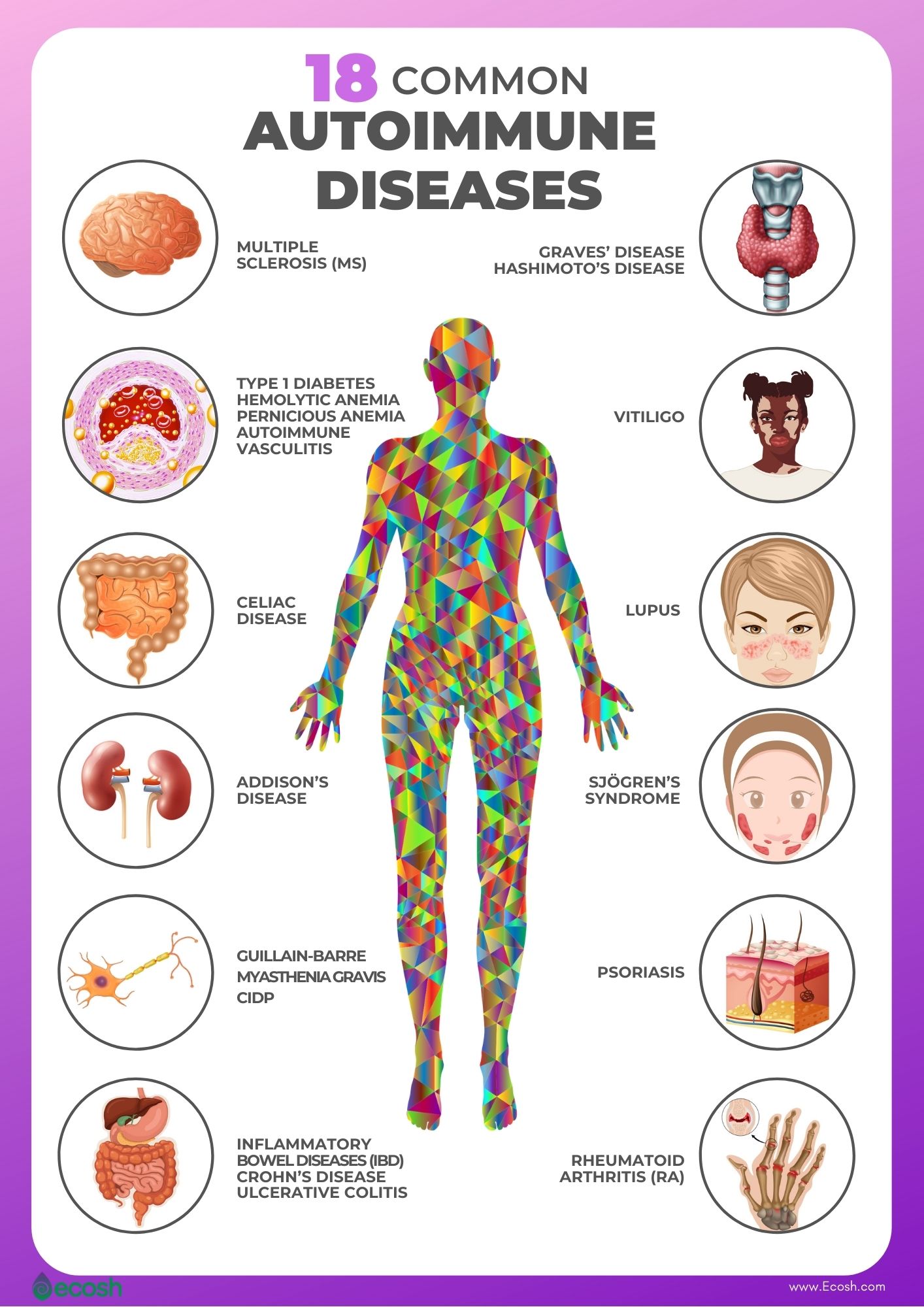
Autoimmune diseases occur when the immune system fails to distinguish between self and non-self entities. Instead of protecting the body, it launches an attack on its own cells and tissues. There are over 80 different types of autoimmune diseases, each with unique characteristics. Some common examples include rheumatoid arthritis, lupus, psoriasis, and Sjögren's syndrome. These conditions can affect any part of the body, including joints, muscles, skin, blood vessels, and internal organs. The exact cause of autoimmune diseases remains unclear, but researchers believe genetic, environmental, and hormonal factors play significant roles in their development.
| Personal Information | Data |
|---|---|
| Name | [Insert Name] |
| Date of Birth | [Insert Date] |
| Place of Birth | [Insert Place] |
| Career | Researcher in Autoimmune Diseases |
| Professional Affiliation | Mayo Clinic |
Rheumatoid arthritis (RA) is one of the most prevalent autoimmune diseases, characterized by chronic inflammation of the joints. The immune system produces antibodies that attach to the linings of the joints, leading to pain, swelling, and stiffness. Over time, this can result in joint deformity and loss of function. Treatment typically involves a combination of medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and disease-modifying antirheumatic drugs (DMARDs). In severe cases, surgery may be necessary to repair or replace damaged joints.
Lupus is another autoimmune disease that affects multiple systems in the body. It often manifests with symptoms such as fatigue, fever, rash, and joint pain. The severity of lupus varies widely among individuals, ranging from mild to life-threatening. Diagnosis can be challenging due to the diverse nature of symptoms and the absence of a single definitive test. Management focuses on controlling symptoms and preventing flare-ups through medication, lifestyle modifications, and regular monitoring by healthcare professionals.
Sjögren's syndrome is an autoimmune disorder primarily affecting the glands responsible for producing tears and saliva. This results in dry eyes and a dry mouth, significantly impacting daily life. While there is no cure for Sjögren's syndrome, treatments aim to alleviate symptoms and prevent complications. Artificial tears, saliva substitutes, and medications to stimulate glandular secretion are commonly prescribed. Additionally, addressing systemic involvement, such as lung or kidney problems, is essential for comprehensive care.
Psoriasis is a chronic autoimmune condition characterized by rapid skin cell growth, leading to thick, scaly patches on the skin. Although primarily a skin disease, psoriasis can also affect the joints, causing psoriatic arthritis. Both conditions require long-term management, involving topical treatments, phototherapy, and systemic medications. Emerging biologic therapies targeting specific components of the immune system have shown promising results in reducing inflammation and improving symptoms.
Autoimmune diseases can also target internal organs, as seen in conditions like type 1 diabetes and Hashimoto's thyroiditis. In type 1 diabetes, the immune system destroys insulin-producing beta cells in the pancreas, resulting in high blood sugar levels. Treatment involves lifelong insulin therapy and careful monitoring of blood glucose levels. Hashimoto's thyroiditis, on the other hand, leads to hypothyroidism due to the destruction of thyroid tissue. Hormone replacement therapy with levothyroxine is the standard treatment to restore normal thyroid function.
Multiple sclerosis (MS) is a demyelinating autoimmune disease affecting the central nervous system. The immune system attacks the protective covering of nerve fibers, disrupting communication between the brain and the rest of the body. Symptoms vary depending on the location and extent of damage, including muscle weakness, coordination difficulties, vision problems, and cognitive impairment. Disease-modifying therapies aim to reduce the frequency and severity of relapses, slowing disease progression and improving quality of life.
Myasthenia gravis is an autoimmune disorder characterized by muscle weakness and fatigue. It occurs when antibodies block or destroy receptors at the neuromuscular junction, impairing signal transmission. Common symptoms include drooping eyelids, double vision, and difficulty swallowing or speaking. Treatment options include anticholinesterase medications, immunosuppressive drugs, and plasma exchange or intravenous immunoglobulin therapy in severe cases.
Addison's disease, also known as primary adrenal insufficiency, results from the immune system attacking the adrenal glands. This leads to insufficient production of hormones such as cortisol and aldosterone, causing symptoms like fatigue, weight loss, low blood pressure, and hyperpigmentation. Hormone replacement therapy is essential for managing Addison's disease, ensuring adequate levels of cortisol and aldosterone to maintain normal bodily functions.
Celiac disease is an autoimmune reaction triggered by consuming gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease ingest gluten, their immune system damages the lining of the small intestine, interfering with nutrient absorption. A strict gluten-free diet is the only effective treatment, allowing the intestinal lining to heal and preventing long-term complications such as osteoporosis and certain cancers.
Dermatomyositis is an inflammatory autoimmune disease affecting the muscles and skin. It causes muscle weakness, particularly in the proximal muscles, along with distinctive rashes on the face, knuckles, and other areas. Treatment involves corticosteroids, immunosuppressive agents, and physical therapy to manage symptoms and improve muscle strength. Early diagnosis and intervention are crucial for preventing irreversible muscle damage.
Familial Mediterranean fever (FMF) is an inherited autoimmune disorder characterized by recurrent episodes of fever and inflammation. These attacks typically affect the abdomen, chest, or joints, causing significant discomfort. Colchicine, an anti-inflammatory medication, is effective in preventing attacks and reducing complications such as amyloidosis. Genetic counseling is recommended for families with a history of FMF to assess risks and plan accordingly.
DiGeorge syndrome, also known as 22q11.2 deletion syndrome, is a congenital condition resulting from improper development of the thymus gland. This leads to reduced T cell production and impaired immune function, making individuals more susceptible to infections. Treatment focuses on addressing specific manifestations, including cardiac defects, hypocalcemia, and developmental delays. Immune system support through vaccinations and prophylactic antibiotics is essential for preventing severe infections.
Burkitt lymphoma is a rare but aggressive form of non-Hodgkin lymphoma associated with immune system dysfunction. It often presents with rapidly growing tumors in the jaw, abdomen, or other areas. Treatment involves intensive chemotherapy regimens, sometimes combined with radiation therapy, aiming to eradicate cancer cells quickly. Early diagnosis and prompt initiation of treatment are critical for achieving favorable outcomes.
Ataxia telangiectasia is a rare genetic disorder affecting the immune system and nervous system. Individuals with this condition experience progressive cerebellar ataxia, dilated blood vessels, and increased susceptibility to infections. Management focuses on supportive care, including physical therapy, speech therapy, and immunoglobulin replacement therapy. Research continues to explore potential therapeutic interventions targeting the underlying genetic defect.
In conclusion, autoimmune diseases represent a complex and diverse group of disorders with significant implications for health and well-being. Advances in medical research and technology have improved our understanding of these conditions, enabling more effective diagnostic and treatment strategies. However, much remains to be discovered about their underlying mechanisms and optimal management approaches. Continued collaboration among scientists, clinicians, and patients is vital for driving progress in this field and enhancing the lives of those affected by autoimmune diseases.