Is universal healthcare truly free? While the term free healthcare is often used, it's important to understand that no system is entirely without cost. Instead, these systems are funded through taxation and government allocation, ensuring access to medical services for all citizens. Brazil stands out as a country where healthcare is defined as a universal right under its Constitution, making it accessible to everyone regardless of their financial status. This bold commitment to public health sets a precedent for nations worldwide.
However, the concept of universal healthcare extends beyond Brazil. Several other countries have implemented similar systems, each with its unique approach and challenges. For instance, Luxembourg introduced its universal healthcare system in 1973, while the Netherlands did so in 1966. New Zealand pioneered such a system back in 1938, and Norway established its framework in 1912. These nations exemplify how long-standing commitments to public health can lead to robust healthcare infrastructures.
| Country | Year Established | Healthcare Type | Website Reference |
|---|---|---|---|
| Brazil | Constitutional Right | Universal Public Healthcare | Brasil Health Ministry |
| Luxembourg | 1973 | Social Security-Based | Luxembourg Health Ministry |
| Netherlands | 1966 | Mixed Public-Private System | Netherlands Health Authority |
| New Zealand | 1938 | Publicly Funded | New Zealand Health Ministry |
| Norway | 1912 | State-Funded | Norwegian Directorate of Health |
In Europe, nearly all countries operate under a universal healthcare system. Although sometimes referred to as free healthcare, it’s more accurate to describe it as taxpayer-supported healthcare. Each nation tailors its approach based on cultural, economic, and political factors. For example, Canada employs a publicly funded, single-payer model, whereas Germany combines mandatory insurance with private options. France balances public provision with supplementary private coverage, reflecting its dual commitment to equity and choice.
The Rekindling Reform initiative delved into the health systems of four key countries—Canada, France, Germany, and Great Britain—to uncover common principles and best practices. Among the findings were ten crosscutting lessons applicable across diverse contexts. One critical insight was the importance of integrating primary care into broader health strategies. Another emphasized leveraging technology to enhance service delivery and patient outcomes. These insights underscore the value of learning from global peers when designing effective healthcare policies.
Twenty-five European countries rely on government-regulated networks of private insurers to deliver universal healthcare. Such arrangements allow flexibility in managing resources while maintaining equitable access. However, they also pose challenges related to cost containment and administrative efficiency. Balancing these competing demands requires careful planning and ongoing evaluation.
Rick Steves highlights the practical aspects of European healthcare systems, noting that despite occasional mischaracterizations as free, these programs function through contributions from taxpayers. Citizens benefit from comprehensive coverage that includes preventive care, hospital stays, and prescription medications. Yet, there remain variations between countries regarding specifics like co-payments or supplemental plans.
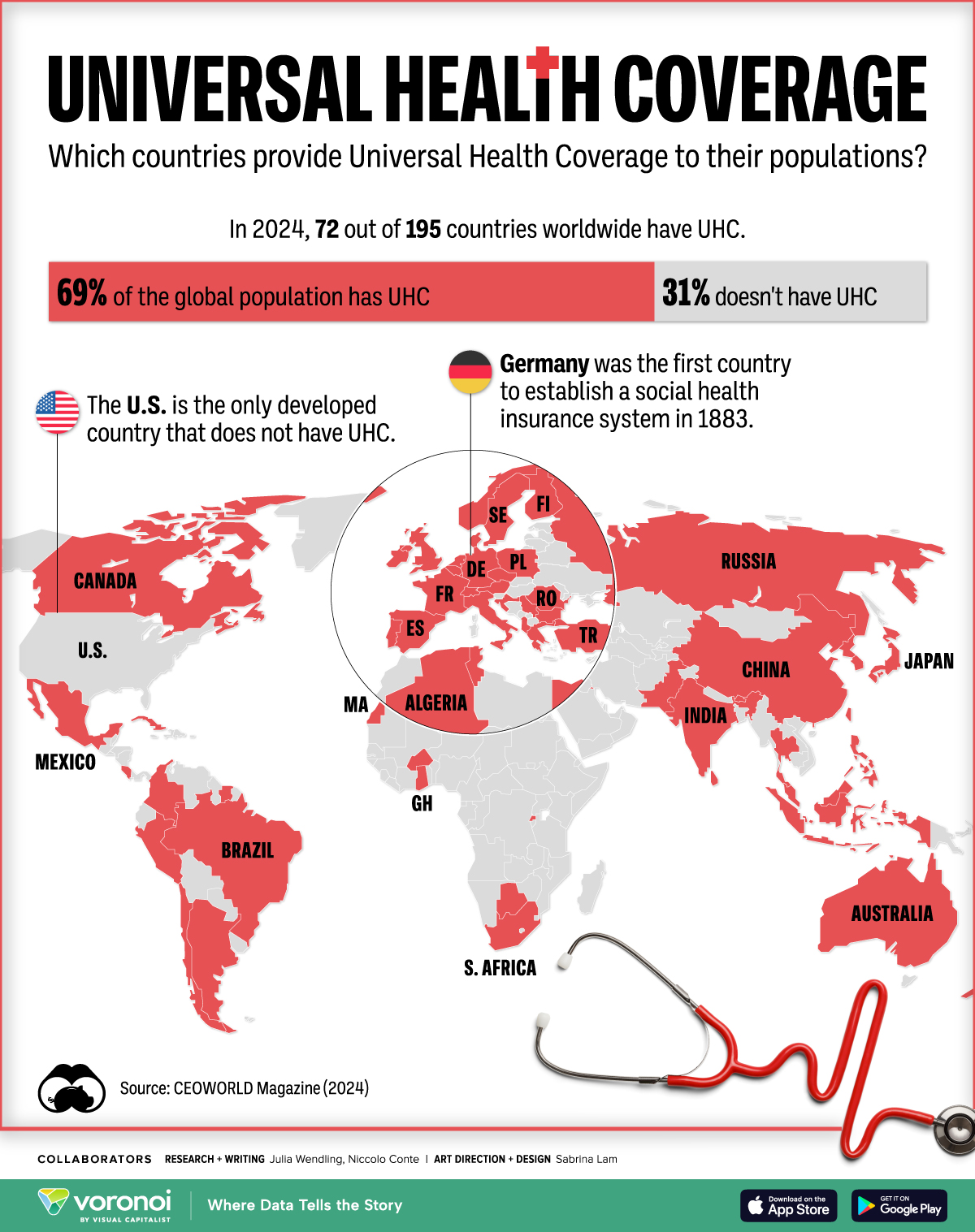
Universal Health Coverage (UHC) represents a cornerstone of sustainable development goals globally. It aims to ensure everyone receives necessary healthcare services without suffering financial hardship. According to WHO fact sheets, implementing UHC offers numerous benefits, including improved population health, reduced poverty levels, enhanced productivity, and greater social cohesion. Achieving UHC necessitates strong leadership, adequate funding mechanisms, skilled workforce development, and reliable data collection systems.
Among the twenty countries offering free healthcare, notable examples include Finland, Sweden, Denmark, Iceland, Austria, Belgium, Switzerland, Portugal, Spain, Italy, Greece, Malta, Cyprus, Slovenia, Croatia, Czech Republic, Slovakia, Hungary, Poland, and Estonia. Each has crafted its version of universal healthcare tailored to local needs and conditions. Despite differing approaches, all share the fundamental objective of providing quality care equitably.
It's worth reiterating that the United States remains an anomaly among developed nations by lacking a fully realized universal healthcare system. Critics argue this absence costs the country trillions annually due to inefficiencies and disparities. As discussions around healthcare reform continue, examining successful international models could inform potential solutions suited to America's context.
Ultimately, understanding universal healthcare involves recognizing both its promise and complexities. By studying various implementations worldwide, policymakers and stakeholders gain valuable perspectives on creating inclusive, sustainable systems capable of meeting populations' evolving health needs.